Table of Contents
|
|
|
Introduction to DACnet
Welcome to DACnet!
This User Guide has been provided to assist you in sending claims electronically. Please give this manual to your office manager and keep it beside the computer. All staff processing claims are encouraged to read the manual carefully. The User Guide contains a list of those insurance companies currently accepting denturist claims electronically with DACnet along with their corresponding ID numbers and processor contact phone numbers. Your software vendor will inform you when additional carriers are to be added to your system. For the most up to date list of carriers and the types of claims they accept please refer to the DACnet website at www.dacnet.ca.
Please ensure that your staff is fully trained on DACnet prior to using the system. Please contact your software vendor to arrange for a training session. This training is only offered by your software vendor. We therefore encourage you to always maintain your support contact with your vendor, so that you can receive all of the DACnet updates regularly.
What is DACnet?
The Denturist Association of Canada in conjunction with the Canadian Dental Association, provincial associations, insurance carriers, network suppliers and system vendors, have established a network that allows you to submit claims and pre-treatment plans electronically (EDI). This network is called DACnet. DACnet provides you with an efficient method of sending information to insurance carriers and reduces the turnaround time for claim payment.
Lost or delayed claim forms will become things of the past, and patient queries regarding procedures and coverage may be answered within minutes! Because dental claims are forwarded to the respective insurance carrier electronically, patients are no longer required to send in their forms.
Processing claims electronically:
- Allows carriers to process them and reimburse patients for the covered portion of their treatment more quickly.
- Eliminates delays caused by late or lost mail.
- Reduces the time it takes for patients to be reimbursed for treatment by half.
How will DACnet affect my computer system?
Your software vendor has made changes to your computer system to allow for the electronic transmission of claim information to claims processors. In order to submit a claim through DACnet, you may be required to enter some additional information that was not previously required. Because the additional details are specific to your computer system, your software vendor will advise you of such changes.
Will there be any change in office procedures?
Since your computer system may require additional information about each patient, it may be necessary to request these details at every patient's first appointment after you begin using DACnet. A sample form currently being used by denturist offices for the purpose of collecting this information is shown in Appendix C. You may wish to use this form, or create your own.
To prevent errors and possible rejection of claims due to invalid information, please remind patients to inform your office of any changes in address, employer, policy number or related information upon arrival for an appointment. You may wish to confirm the insurance information before submitting a claim.
Before the patient leaves the office, you will receive a Claim Acknowledgement or Explanation of Benefits from the claims processor. The form must be given to the patient prior to his/her leaving the office as a receipt that their claim was sent.
Rules and Regulations
Please begin using DACnet on your assigned start date. Although it may not always be possible to begin right away, please make an effort to send claims electronically as soon as you are able.
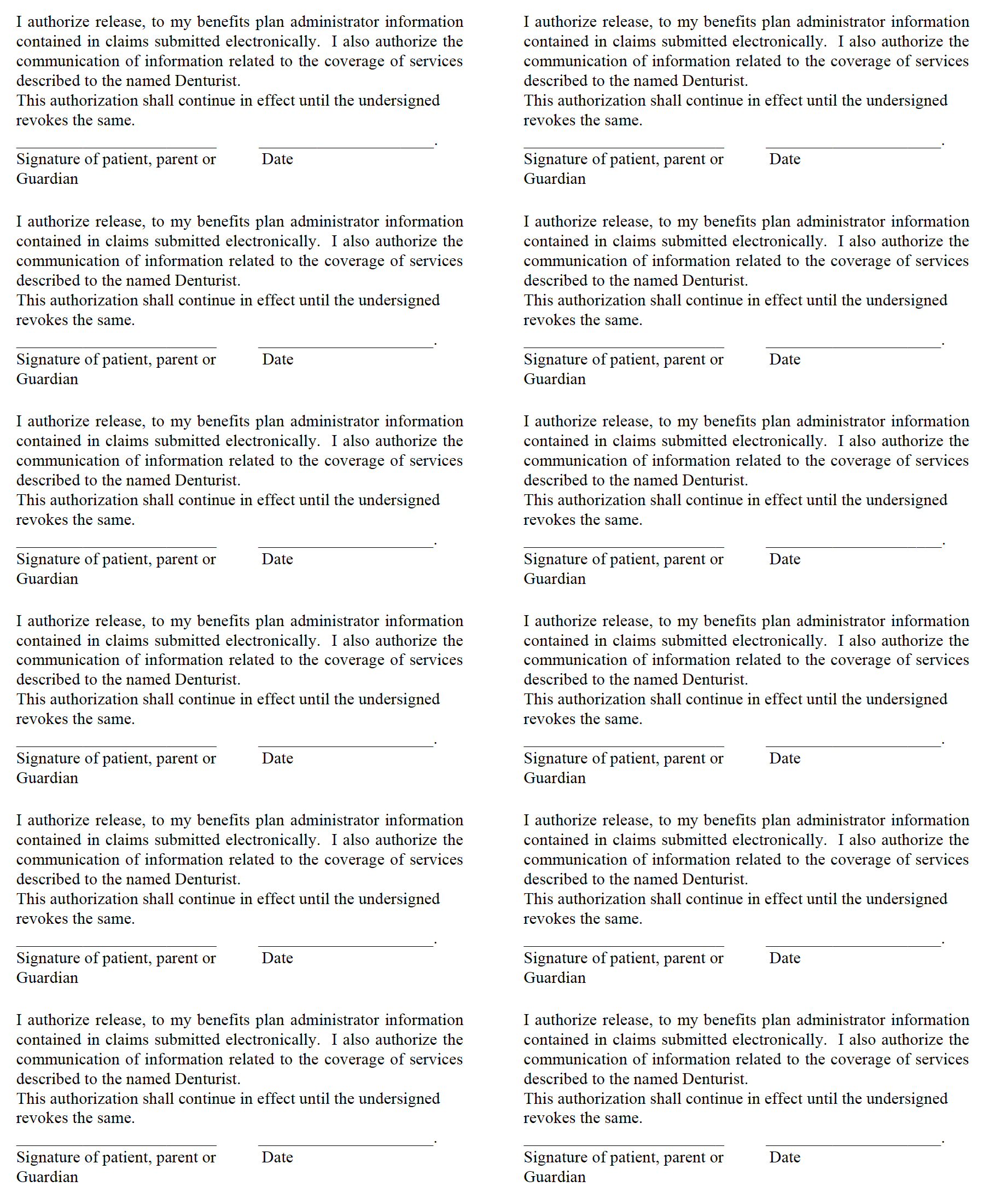
You are required to obtain patient signatures authorizing your office to submit their claims electronically. Additional signatures must also be obtained for those patients for whom you accept assignment of benefits. Original copies of the patient's authorization must be kept on file for three years. Please note that a parent or guardian must sign on behalf of the children under the age of 18.
For each patient participating in DACnet the following wording should accompany the signature:
I authorize release to my benefits plan administrator information contained in claims submitted electronically. I also authorize the communication of information related to the coverage of services described to the named denturist. This authorization shall continue in effect until the undersigned revokes the same.
Signature of patient, parent or guardian Date:
For each patient for which you accept assignment of benefits, the following wording should accompany the signature:
I hereby assign my benefits, payable from claims submitted electronically, to and authorize payment directly to him/her.
This authorization shall continue in effect until the undersigned revokes the same. Signature of subscriber Date:
Sample label forms that may be photocopied for this purpose can be found in Appendix E.
In order to submit claims through DACnet, your office requires insurance information that you may not have on file. You may wish to ask your patients to complete a standard information form so that you have all the necessary details on hand. A Patient Information Form can be found in Appendix C.
It is important that your office maintains patient information records, including address information. To ensure that cheques are appropriately mailed by insurance carriers to patients, your office should confirm patient information each time a patient visits your office. If the patient information has changed, you must update the information in your software.
Electronic Submission of Aged Claims
While it is expected that all claims will be transmitted on the date of service, problems may arise which do not allow for the transmission of the claims until a later date. Please refer to Appendix B – DACnet Networks & Insurance Carrier Information for details on DACnet insurance carriers including: age limits, policies and supported transactions. Note: claims older than the insurance carrier age limit must be printed and cannot be transmitted electronically.
Explanation of Benefits (EOB) and Claim Acknowledgement
It is a mandatory requirement that a copy of the EOB be printed and given to the patient in all cases where an EOB is received. This is the patient's receipt for the claim sent. The printing of an office copy of the EOB is at the discretion of the office.
Subscribing a denturist to DACnet
A DACnet Subscription Agreement must be completed in order for the denturist to be added to the DACnet system. The DACnet Subscription Agreement details the terms and conditions regarding the application for, and the terms and conditions regarding the use of DACnet. Every denturist in a DACnet office who plans to submit claims in his or her name must read and accept these terms and conditions before accessing DACnet. Each participating denturist must complete a separate agreement and pay a separate subscription fee.
instream CLAIMS
instream CLAIMS is one network which allows offices to send denturist claims to insurance companies using the Internet. For additional information on instream CLAIMS and applicable fees go to the instream website at www.instreamcanada.com.
TELUS HEALTH
TELUS Health is the other (free) network which allows offices offices to send denturist claims to insurance companies using the Internet. This network uses internet communication software called CCD-WS and your software vendor will need to configure your system accordingly.
How and when to advise DACnet of office information changes
It is important to advise the DACnet Helpdesk at 1-877-832-2638 immediately of any office information changes as claims processors and networks require this information to ensure successful claims transmission. If the third party companies are unaware of such changes, transmission errors might occur.
Types of office changes/updates that require DACnet notification
Listed below are the types of changes that require DACnet notification:
- Subscribing a denturist to DACnet
- Change of DACnet office address information
- Addition or deletion of denturist to a DACnet office
- Change in office practice management software
- Addition or closing of a DACnet office
- Prohibited Practices
- Use of non-certified software to submit claims and predeterminations through DACnet. Contact the DACnet Help Desk if you have any questions concerning your software. Refer to the DACnet website at www.dacnet.ca for a list of certified DACnet software vendors
- Attempts to access services other than those described in this User Guide.
- Any other fraudulent practices related to the use of DACnet.
- Sending claims under another denturist’s Unique ID Number.
- Sending claims from another denturist’s patients under your Unique ID Number.
Failure to comply with the preceding provisions will result in termination of services provided by the networks.
Claims
Real Time Claim Processing
Real time processing means that when you submit a claim, the claims processor will adjudicate it and send a response back to you immediately (approximately 20-40 seconds).
An Explanation of Benefits (EOB) is returned for a claim that is adjudicated in Real time. However, a Claim Acknowledgement (CA) may be sent back if the insurance company chooses to look into the claim further.
In some instances, a claim adjudicated in Real time may be rejected due to errors. If this occurs an error message will be displayed on your screen. Correct the error(s) and resubmit the claim. If still unsuccessful, contact your software vendor for assistance.
Batch Processing
Batch processing means that the insurance carrier will adjudicate all claims at a predetermined time rather than on an as received basis. The claim will usually be adjudicated later in the day or overnight.
A Claim Acknowledgement is always returned for a claim that is received for batch processing. Once the insurance carrier performs adjudication, an Explanation of Benefits (EOB) will be sent to the patient by mail. Or, if the payment is assigned, the EOB will be returned electronically or by mail to your office. It is important that you check your mailbox frequently in order to receive responses from the insurance carriers.
Further information regarding Claim Acknowledgements may be found on page 10. For more details on accessing your mailbox, please refer to the section, "Request for Outstanding Transactions" on page 17.
Pretreatment plans are always batch processed. A message will be displayed on your computer screen advising you that the pretreatment plan was received successfully. The claims processor's approval or denial of the pretreatment plan will be sent by mail to the insured. Please refer to the section on Pretreatment Plans on page 18 for more information.
To Submit a Claim
SEND ONLY VALID CLAIMS; do not attempt to test the system by sending invalid claims.
All claims must be sent under the denturist’s name that is providing the service.
Enter the information required for a claim as defined by your computer system. Confirm that information regarding the insured/patient is correct. Follow the instructions supplied by your software vendor.
Note: All procedures or treatments rendered for a single patient are to be submitted as one claim on the day of treatment. The number of performed procedures permitted in a claim is between 1 - 7. If more than 7 procedures are required, a second claim can be sent for the balance of the procedures. The claims processor will not adjudicate late claims electronically. Offices must not submit the same claim twice.
If the claim is sent successfully, you will receive an Explanation of Benefits for claims processed in Real time, or a Claim Acknowledgement if the claim is processed in Batch mode. These forms should print automatically at your office. If this is not the case, contact your software vendor.
When a third party adjudicates a claim in Real time, the resulting EOB is returned electronically to you shortly after claim submission. One EOB is printed for an unassigned claim. For an assigned claim, your computer system might print two EOBs, one for you and one for the patient, or only one EOB for the patient. You may also contact your software vendor to arrange for one or more printouts to be generated from your system.
The Explanation of Benefits or Claim Acknowledgement must be given to the patient before he or she leaves the office. Patients must always receive this as a receipt of the procedures performed prior to leaving the office. Inform your patient that any questions regarding the benefit calculation should be directed to the claims processor. A cheque will be mailed to the insured or for assigned benefits, directly to the denturist. A sample EOB form is shown on the next page.
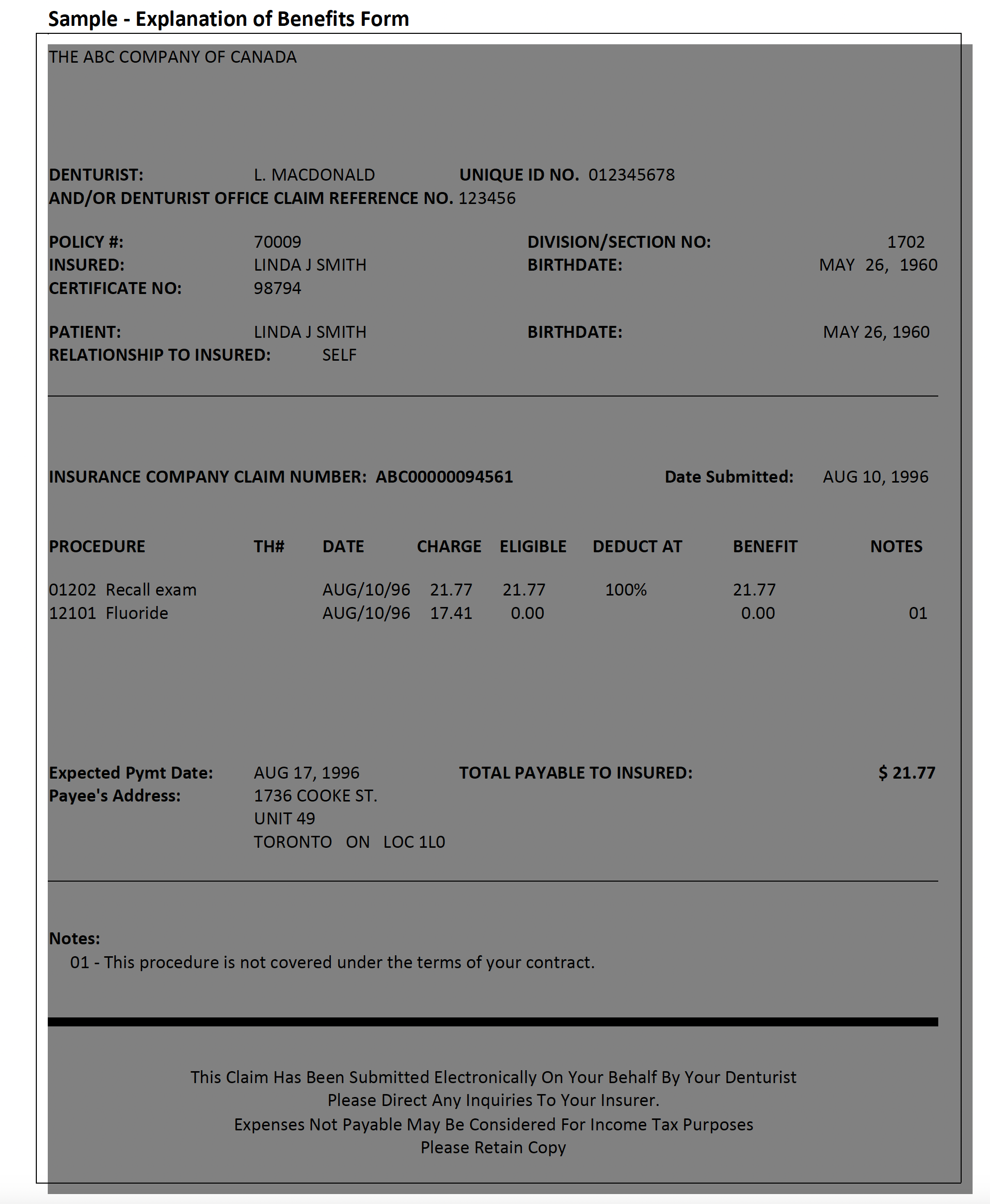
Explanation of Benefits Form Headings
The headings on the EOB are described below:
|
HEADING |
DESCRIPTION |
|
Denturist |
Name of Denturist Providing Service. |
|
Unique ID No. |
9-digit provider ID number assigned to the denturist providing the service. |
|
And/or Denturist Office Claim Reference |
A sequential number identifying the claim submission, which is generated automatically by your computer system. |
|
Policy # |
The patient's insurance policy number. |
|
Division/Section No. |
The division or section number related to the policy number, if applicable. |
|
Insured |
The insured's name. |
|
Birth date |
The insured's birth date. |
|
Certificate No. |
The insured's identification number. |
|
Patient |
The patient's name. |
|
Birth date |
The patient's birth date. |
|
Relationship To Insured |
The patient's relationship to the insured. |
|
Claim No. |
The third party's claim reference number, if applicable. |
|
Date Submitted |
The date that the claim was submitted through DACnet. |
|
Procedure |
The denturist code submitted for the claim, or the procedure code inserted by the third party. Note: In some cases, a procedure code submitted might not be the one that is paid under the insurance policy. The EOB will include the covered procedure code. For insurance carrier inserted procedure codes, a note may refer back to the original procedure line number. This situation is likely to occur |
|
Th # |
The tooth number, if applicable. |
|
Date |
The date of service. |
|
Charge |
The total fee charged for the procedure. |
|
Eligible |
The amount eligible for payment. |
|
Deduct |
The deductible associated with the procedure. If the claims processor |
|
At |
The percentage insured. |
|
Benefit |
The benefit amount payable. |
|
Notes |
Note number(s) referring to the descriptions of procedures listed at bottom of page, if applicable. |
|
Expected Pymt Date |
The expected payment date. |
|
Total Payable To Insured/Provider |
The total amount payable to the insured, or to the denturist if the claim is assigned. |
|
Payee's Address |
The payee's address. |
|
Notes |
Text related to the note number(s) beside procedure lines, if applicable. |
Claim Acknowledgement
When a claim cannot be adjudicated in Real time, a Claim Acknowledgement is returned to you. For an unassigned claim, an EOB will be mailed to the insured. For an assigned claim, an EOB may be returned to your office electronically.
If an EOB is forwarded electronically, you will be able to access and print the EOB from your mailbox. Please refer to Request for Outstanding Transactions on page 17 for further instruction on this procedure.
It is mandatory that a copy of the Claim Acknowledgement be given to the patient before he or she leaves the office. This form provides the patient with a record of the claim, which you submitted to the claims processor on their behalf. The printing of the claim acknowledgement for office use is at the discretion of the office.
If the claim is rejected, you will receive an error message on your computer screen or printer explaining the reason for rejection. Correct the error(s) and resubmit the claim.
Note: A claim that is not adjudicated in Real time may later be rejected during Batch processing. If this situation occurs, the claims processor will contact either the insured or your office.
If no response is received for the claim, check your mailbox later for an EOB or Claim Acknowledgement. If an EOB or Claim Acknowledgement cannot be retrieved, resubmit the claim.
A sample Claim Acknowledgement is shown on the next page. Note that the format of a Claim Acknowledgement may differ slightly because it might be combined with the patient's walkout bill produced by your computer system. A Claim Acknowledgement reflects the submitted amount only: the amount payable may differ.
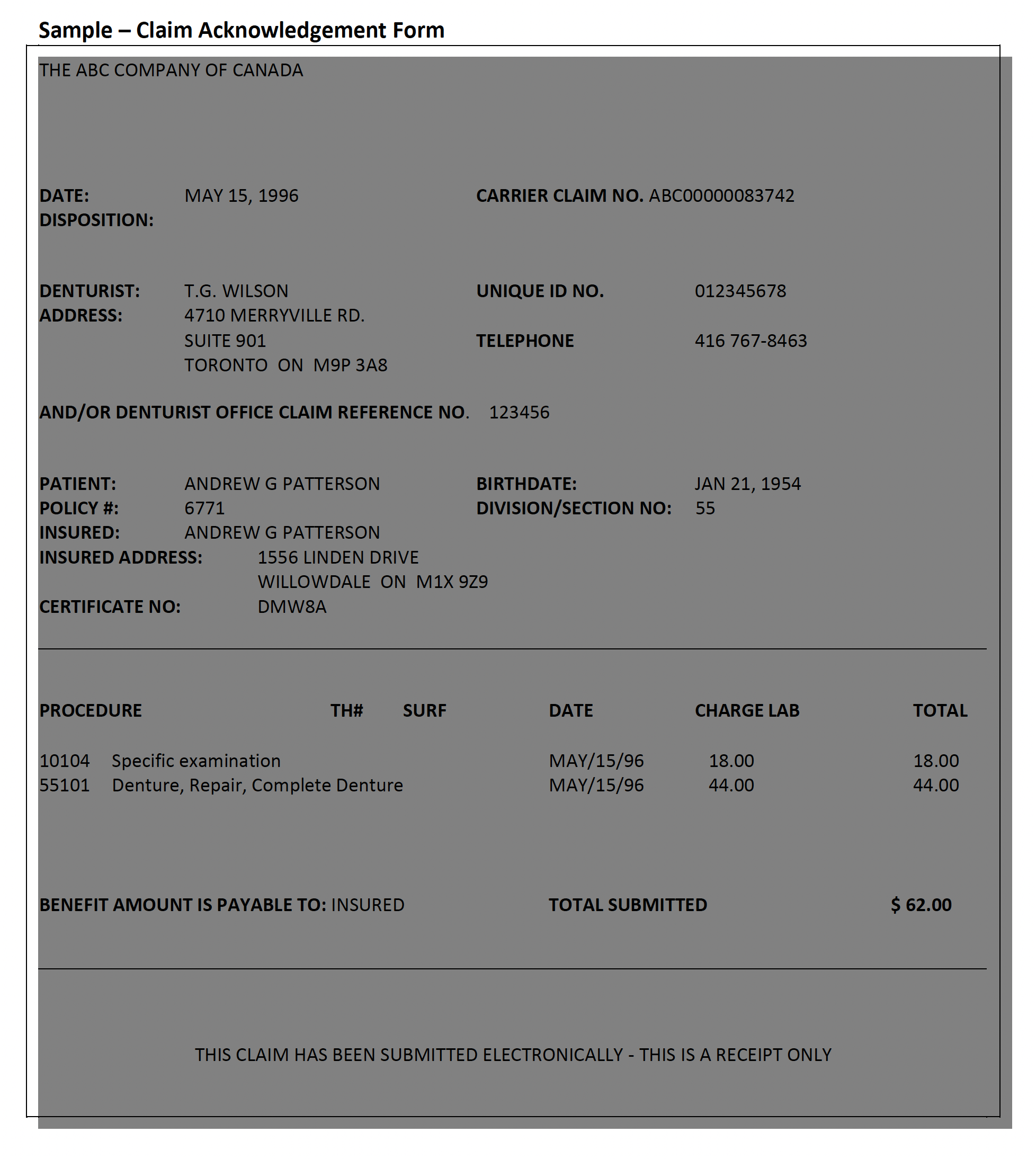
Acknowledgement Form Headings
The headings found on the sample Claim Acknowledgement are described as follows:
|
HEADING |
DESCRIPTION |
|
Date |
The date that the Claim Acknowledgement was printed. |
|
Carrier Claim No. |
The claims processor's claim reference |
|
Disposition |
A message regarding the claim transaction, if applicable. |
|
Denturist |
Name of denturist providing service. |
|
Address |
The denturist's address. |
|
Unique ID No. |
9-digit provider ID number assigned by the CDA, to the denturist providing the service. |
|
Telephone |
The denturist's telephone number. |
|
Office Claim Reference No. |
A sequential number identifying the claim |
|
Patient |
The patient's name. |
|
Birth date |
The patient's birth date. |
|
Insured Address |
The insured's address. |
|
Policy # |
The insured's policy number. |
|
Division/Section No. |
The division or section number related to the policy number, if applicable. |
|
Insured |
The insured's name. |
|
Certificate No. |
The insured's identification number. |
|
Procedure |
The procedure code submitted for the claim. |
|
Th # |
The tooth number, if applicable. |
|
Surface |
The tooth surface, if applicable. |
|
Date |
The date of service. |
|
Charge |
The charge for the procedure. |
|
Lab |
The lab fee charged for the procedure. |
|
Benefit Amount is Payable To |
The benefit payee. |
|
Total Submitted |
The total charges submitted for the claim. Note: The amount payable may differ |
Employer Certified Claims
Some claims must be signed and certified by the insured's employer before being processed by the claims processor. These claims cannot be adjudicated in Real time.
For this type of claim, an Employer Certified Form will be returned to you shortly after claim submission. This form will advise the insured that an authorized signature must first be obtained, following which the Employer Certified Form can be mailed to the claims processor.
Some employers require forms with slightly different information. In this situation, simply staple the Employer Certified Form to the patient's form.
A sample Employer Certified Form is shown on the next page.
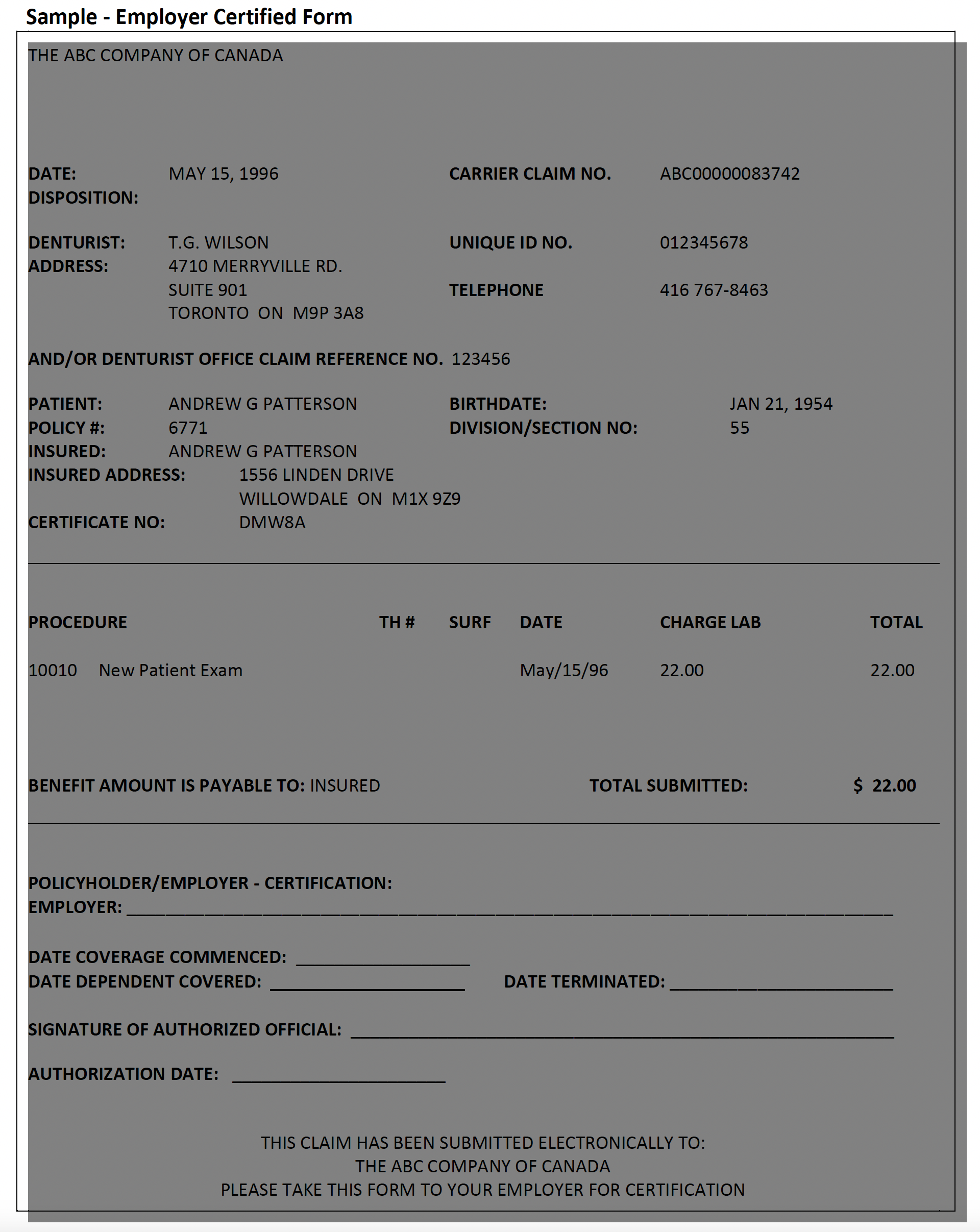
Employer Certified Form Headings
The headings on the Employer Certified Form are similar to those used on the Claim Acknowledgement, with the exception of an additional area to be completed by the insured's employer. The "Policy holder/Employer Certification" section of the form is described below:
|
Employer |
The employer's name. |
|
Date Coverage Commenced |
The initial date of coverage for the insured. |
|
Date Dependent Covered |
The initial date of coverage for the insured. |
|
Date Terminated |
The last day of insurance coverage. |
|
Signature Of Authorized Official |
The signature of the person certifying that the insured's information is correct. |
|
Authorization Date |
The date that the claim was certified. |
Reversing a Claim
A claim submitted in error may be voided by performing a claim reversal. A claim reversal voids all procedures that were part of the original claim.
A claim may only be reversed using DACnet on the same day that it was submitted. If you notice that a claim is invalid on a following day, notify the claims processor either by phone or by mail, quoting the carrier claim number and the office claim reference number as shown on the EOB or Claim Acknowledgement as soon as possible.
To reverse a claim:
Enter the information required for a claim reversal as defined by your computer system. Be sure to indicate the same carrier claim number and office claim reference number as shown on the Claim Acknowledgement or Explanation of Benefits. Follow the instructions supplied by your software vendor.
If the reversal is successful, you will receive a message on your computer screen advising you of this.
If the reversal is rejected, you will receive an error message on your computer screen explaining the reason for rejection. If possible, correct the error(s) and resubmit the claim reversal. If the reason for rejection cannot be corrected, notify the third party either by phone or by mail that the original claim was invalid.
Pended Claims/Request for Outstanding Transactions
The denturist office should initiate the Request for Outstanding Transactions regularly. This mailbox is referred to as the pended claims file in Version 2. It contains responses from the claims processors that are sent after the Real time transaction takes place. Please note that this feature is available through TELUS Health Solutions - Group A and instream only. Assignment
practices tend to have more EOBs sent to their mailbox, and should therefore check their mailbox daily. The types of responses that are placed in the mailbox for the denturist are outlined below:
- EOB Response
- Claim Acknowledgement
- Outstanding Transaction Response
- Predetermination EOB
- Predetermination Acknowledgement
- E-mail Response
Occasionally, a claim or predetermination is submitted and the denturist receives a response from the network. This occurs when the network accepts the claim on behalf of the claims processor. Denturists can recognize a response from a network by the message "Transaction Received by Network. Check Mailbox Tomorrow".
It is important for the denturist to check the mailbox after receiving this message, as there might be an additional message from the claims processor. The third party may also send a claim/predetermination rejection to the mailbox. The denturist needs to receive this message to know to resubmit the claim.
The claims processor might also send an Explanation of Benefits as a follow-up response to the original Claim Acknowledgement. This will only occur for assigned claims, once the adjudication process has been completed by the carrier.
If the connection between the office and the network is lost during transmission, a denturist should check their mailbox. If after the claim was sent no response was received and if the claim was received by the network or claims processor, a response will later be found in the mailbox.
Check your mailbox regularly. This will ensure that all responses are received. If you have any questions regarding how to complete this transaction, please contact your software vendor for assistance.
Pre-treatment Plans (Predetermination)
A pre-treatment plan is used to submit information to the third party regarding planned treatment so that the patient is aware of his or her portion of the overall cost. DACnet allows you to submit pre-treatment plans electronically, thereby reducing turnaround time and preventing lost and/or misplaced forms. Occasionally, additional information related to the pre-treatment plan, such as x-rays, may need to be mailed to the claims processor.
To Submit a Pre-treatment Plan
Enter the information required for a pre-treatment plan as defined by your computer system. Ensure that all information for the patient/insured is correct. Follow the instructions provided by your software vendor.
If the pre-treatment plan is sent successfully, you will receive a message on your computer screen advising you of this. If the claims processor is able to evaluate the pre-treatment plan in Real time then a Pre-treatment EOB will be printed. If not, then the third party response will indicate that either a Pre-treatment EOB will be sent electronically at a later time, or the review of the pre-treatment plan will be mailed.
Coordination of Benefits
Coordination of Benefits for Version 2
The Canadian Life and Health Insurance Association provide these guidelines for Coordination of Benefits:
If the patient has coverage for denturist services, their insurance carrier is the primary carrier.
If the patient is a dependent, the insurance carrier for the parent (or covered person) with the earlier birth date in the calendar year is used as the primary carrier. For example, if Mrs. Smith's birth date is February 14 and Mr. Smith's birth date is August 11, then the insurance carrier for Mrs. Smith is the primary carrier for the Smiths' dependent children.
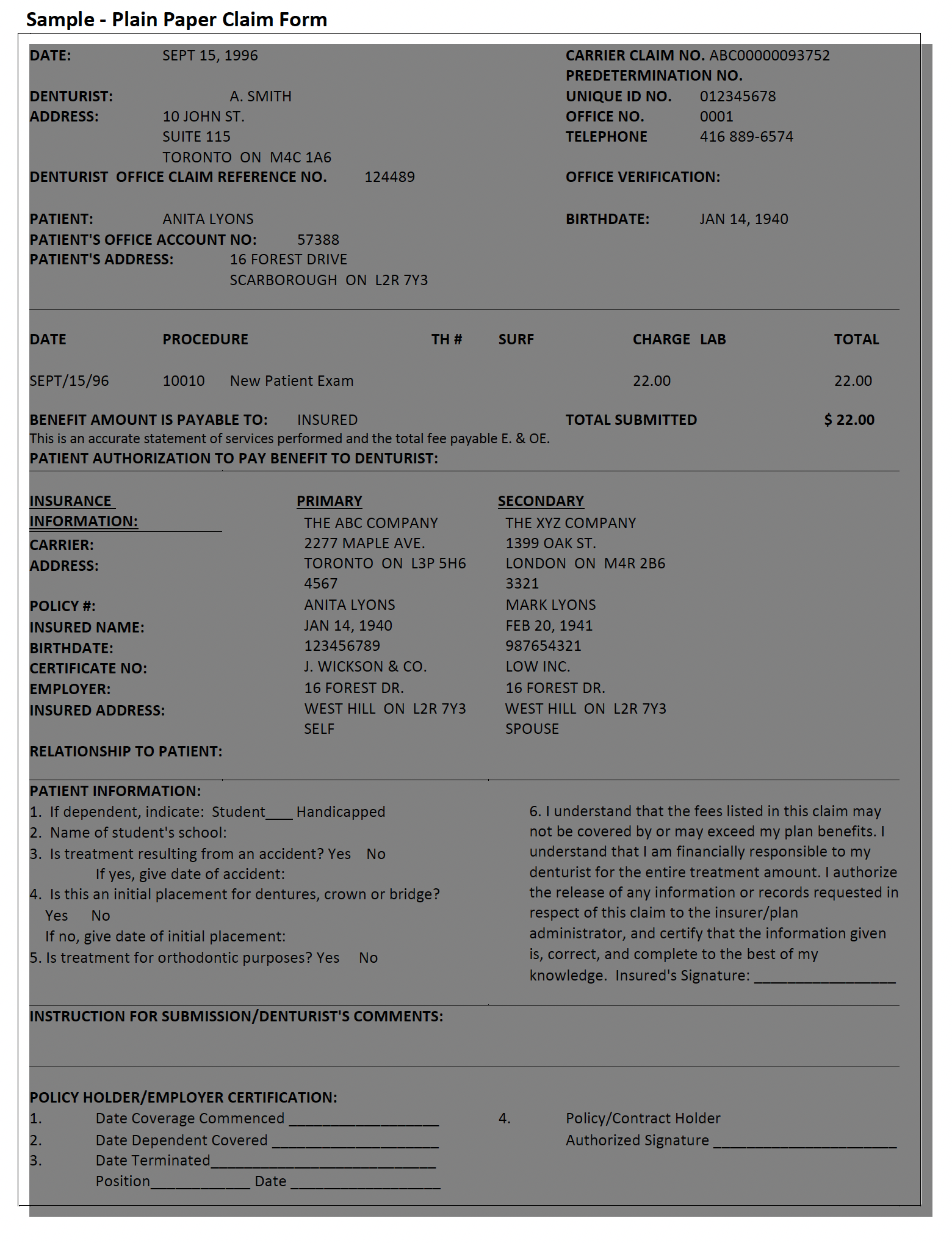
Both an EOB and a claim form will be printed if a claim involving COB is adjudicated in Real time. The claim form may be a standard claim form or, if your office has only one printer, a "Plain Paper Claim Form" as shown on the next page. The headings on this form are similar to those found on the standard claim form.
Coordination of Benefits for Version 4 Claims
Claims should first be transmitted through DACnet for the primary carrier. An EOB will be printed for the primary carrier; the handling of a COB will depend upon several factors:
- If the secondary coverage is adjudicated by the same party as the primary coverage, such as when the primary and secondary carriers are the same, then a second EOB for the secondary carrier may be printed.
- If the secondary carrier accepts COB Claim Transactions then a claim will be transmitted to the secondary carrier, including a copy of the EOB from the primary carrier. An EOB from the secondary carrier will be printed if the secondary claim is adjudicated in Real time.
- If the secondary carrier does not accept COB Claims then a claim form will be printed for the secondary coverage.
** Please see http://dacnet.ca/pdf/coordinationOfBenefitsE.pdf for more information
Summary Reconciliation
(This option is available through Version 4.0 only)
A summary reconciliation is retrieved, from networks that support this feature, to confirm the claim settlement details which have been indicated on EOBs received on a specified business day. When networks provide settlement for a day's claims via electronic funds transfer this reconciliation may serve as a detailed backup to the amount settled.
To Submit a Summary Reconciliation Request:
- Follow the instructions supplied by your software vendor regarding submitting a request for summary reconciliation. Ensure that you correctly enter the date for which the reconciliation is requested.
If the request is sent successfully, you will receive a message on your computer screen advising you of this. Your software will either print the reconciliation information or store it to be used in clearing an EFT payment.
If the request is rejected, you will receive an error message on your computer screen explaining the reason for the rejection. Correct the error(s) and resubmit the request.
Payment Reconciliation
(This option is available through Version 4.0 only)
Payment reconciliation is retrieved, from networks or carriers that support this feature, to provide the claim settlement details for claims that have been settled with a bulk payment.
To Submit a Payment Reconciliation Request:
- Follow the instructions supplied by your software vendor regarding submitting a request for payment reconciliation. Ensure that you correctly enter the settlement date for which the reconciliation is requested.
If the request is sent successfully, you will receive a message on your computer screen advising you of this. Your software will either print the reconciliation information or store it to be used in clearing the bulk payment. If the request is rejected, you will receive an error message on your computer screen explaining the reason for the rejection. Correct the error(s) and resubmit the request.
E-mail Transmissions
Version 4.0 of DACnet will allow carriers and networks to send messages to your office regarding issues related to the electronic claims submission process. This will greatly assist the transfer of information needed for efficient claims adjudication and provide a means for the networks to inform you of any changes or problem areas.
Attachments
Attachments may now be sent with Version 4.1 only; these attachments may consist of XRAYS or other oral images, or documents describing treatment plans or other pertinent information.
The Attachment message is an optional message for application software. A vendor does not need to support this message type if they choose not to. Any supporting material for a claim needs to be physically mailed if the carrier or the application software does not support this message type.
Image Specifications:
Black & White: XRAYS and other black and white images must be scanned in 8 or 16Bit Greyscale at a resolution between 150 DPI and 300 DPI inclusive.
Colour: Intra-oral and other images, pictures, must be scanned in 16, 24 or 32bit Colour at a resolution between 300 DPI and 600 DPI inclusive.
Care must be taken to ensure that only originals are scanned to ensure optimum digital image quality and thereby usability of the image.
Document must be submitted in ASCII text or Microsoft Word formats.
Carrier and Network Information
At times, you may require assistance in solving problems related to DACnet. The following offer suggestions to address particular concerns.
Networks & Insurance Carriers that support DACnet
The format for entering numbers on your computer system differs by insurance carrier. The details on the types of transactions supported by the Networks & Insurance Carriers are attached in Appendix B. This information is available on the DAC website at www.dacnet.ca.
DACnet Networks
Networks such as TELUS Health Solutions and instream provide your office with the ability to submit claims electronically. Pacific Blue Cross is a network operating in British Columbia.
Alberta Blue Cross and Manitoba Blue Cross are also networks facilitating receipt and adjudication of electronic claims.
Problems with Connecting to the Network
If you have problems with connecting to the network, this is likely a software or hardware problem and should be addressed to your software vendor. A list of certified DACnet vendors is available on the DACnet website at: www.dacnet.ca.
Frequently Asked Questions about DACnet
Claims are not transmitting through DACnet. What should be done?
Contact the DACnet Help desk at 1-877-832-2638 to confirm your start date, office number and unique number. Contact the appropriate network, depending on which carrier is not transmitting. If the network has not received your claim, contact your software vendor for support.
Instream users may access the instream web portal to check on the status of a claim, or call the instream help desk at 1-855-521-1121 Monday to Friday. Note that instream users can also
temporarily allow their software vendor to access the instream transmitted claims status information page to assist in problem resolution.
The denturist office information has been changed (address, phone number or software vendor). What should be done?
To update your DACnet file you may:
- Call the DACnet Help Desk at 1-877-832-2638 between 9 a.m. and 5 p.m. (EST) Monday to Friday.
- Email
This email address is being protected from spambots. You need JavaScript enabled to view it. - Complete the office update form at http://dacnet.ca/pdf/update_denturist_office_informationE_ApFillable.pdf
What if a patient deals with a claims processor that is not participating in DACnet?
The insured should continue to submit his or her claims on paper.
Can I send a claim after normal business hours or on weekends?
Yes, you will receive a Claim Acknowledgement shortly after submitting the claim.
DACnet claims may be transmitted 24 hours a day, seven days a week, including holidays. If the carrier system is not available, the system will acknowledge receipt of the claim, and forward the claim to the carrier system when it becomes available.
What should I do if a claim or predetermination is rejected?
You will receive an error message on your screen explaining the reason for rejection. Correct the error(s) and resubmit the claim or predetermination, using a new claim reference number.
If your system does not accept the changes, call the applicable carrier. If you receive an error that you don't understand, call: 1-877-832-2638 or email
Why did I receive a message advising me that I am not authorized to access DACnet?
If you recently subscribed to DACnet, you should contact DACnet to verify that you and the claims processors are using the same identification numbers, call: 1-877-832-2638 or email
Can I reverse a claim that was submitted yesterday?
No, a claim reversal can only be performed on DACnet on the same day the claim was submitted. Call or write the claims processor, quoting the claim reference number shown on the Explanation of Benefits or Claim Acknowledgement, and inform the Claims Department of the error.
If the office staff does not know how to do a claim reversal, they should contact their insurance carrier for information. If the claim cannot be reversed on the same day due to errors, the office must send a manual claim form with a letter referencing the initial claim to the insurance company.
I tried to reverse a claim, and received a message asking me to try again later. What happened?
The claims processor was unable to handle your request for a claim reversal at the time it was submitted. Try to reverse the claim again later in the day. If you are unable to reverse the claim on the same day, follow the procedures for sending a claim reversal manually.
I received a message stating "Network error, please resubmit claim." Is there something wrong with my computer system?
No, this message indicates that there was a temporary transmission problem. Try submitting the claim again.
How should I notify the claims processors of the address change when I move my office?
To change your office information (address, telephone number, etc.)
- Call the DACnet Help Desk at 1-877-832-2638 between 9 a.m. and 5 p.m. (EST) Monday to Friday.
- Email
This email address is being protected from spambots. You need JavaScript enabled to view it. - Complete the office update form at http://dacnet.ca/pdf/update_denturist_office_informationE_ApFillable.pdf
How do I change a patient's address?
Update the information on your computer. The new address will be reflected on subsequent claims.
I received a message stating "Error code ". What does this mean?
Contact your software vendor to request that descriptions be added to these error codes. A list of error codes can also be found in Appendix D.
I received an error message and have no idea where the problem lies.
In the event that office staff cannot correct an error message, Call the DACnet Help Desk at 1- 877-832-2638 between 9 a.m. and 5 p.m. (EST) Monday to Friday or Email
The icon (or window B, depending on the software) is not giving me the option to use CDAnet. Why not?
Either the denturist record in your software is not configured to allow electronic claims or the carrier record in your software does not indicate support for electronic claims.
Contact the software vendor in order to update the information found in their software to correct the above issue.
Where do I receive updates?
Your software vendor supplies updates to your practice management software. Updates such as new carrier, carrier networks and supported transactions types can be obtained through the networks and DACnet.
I'm getting an invalid carrier ID code. What does that mean?
It means that the ID number you have programmed for the insurance company is incorrect. Verify the information and make any necessary changes. If you're unsure on how to change this information, contact your software vendor for additional help.
I'm receiving the error code "Datapac not responding." What does that mean?
This error does not apply to instream users.
DATApac has been phased out by TELUS Health Solutions. Offices can contact the TELUS Help Desk at 1-866-272-2204.
What is the difference between Batch Mode and Real Time?
Batch processing means that the insurance carrier will adjudicate all claims at a predetermined time rather than on an as received basis. The claim will usually be adjudicated later in the day or overnight.
Real time processing means that when you submit a claim, the claims processor will adjudicate it and send a response back to you immediately (approximately 20-40 seconds).
Do patients have to sign anything to transmit claims electronically?
Yes, a patient has to sign an authorization giving the office permission to transmit his or her claims electronically. The authorization information can be found on page 3 and the labels are on page 36.
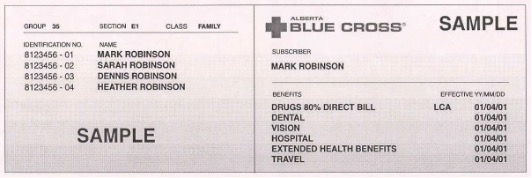
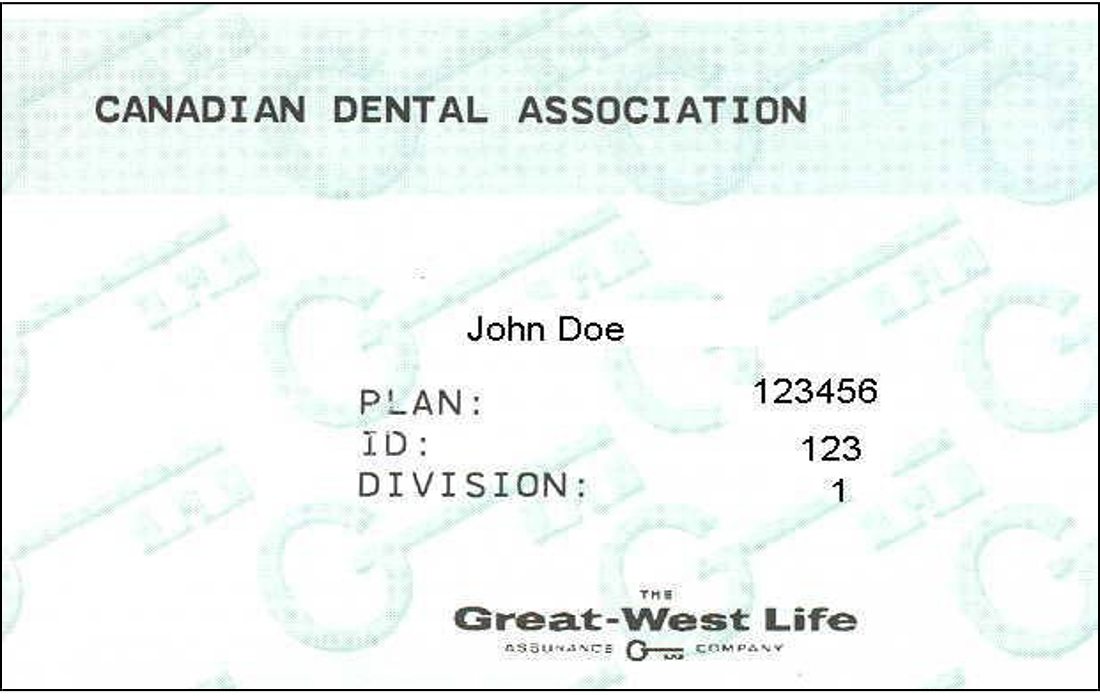
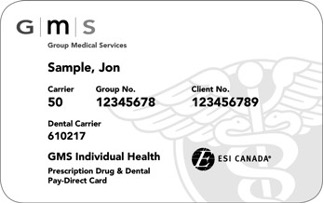
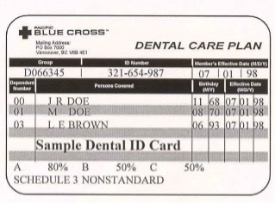
Appendix A – Sample Insurance Cards
Some of the terms used on claim forms may be unfamiliar to you. Policy number may also be referred to as group number, plan number and control number. Division number is also called section number, suffix number and unit number. Subscriber ID is also known as certificate number, SIN, employee ID and cardholder ID.
Below are sample insurance cards.
The TELUS | Assure Card (formerly the BCE Emergis or Emergis Card)
Some patients may carry a plastic or paper card identified as the TELUS | Assure Card (formerly the BCE Emergis or Emergis card). These cards may have different artwork (depending on the insurance carrier and/or plan sponsor), however, all cards will contain the same information. The TELUS | Assure logo will appear on all cards to allow easy recognition.
As the TELUS | Assure Card is issued for both drug and dental plans, some of the information on the card may not apply to denturist claims.
A sample of the TELUS | Assure Card is illustrated below:
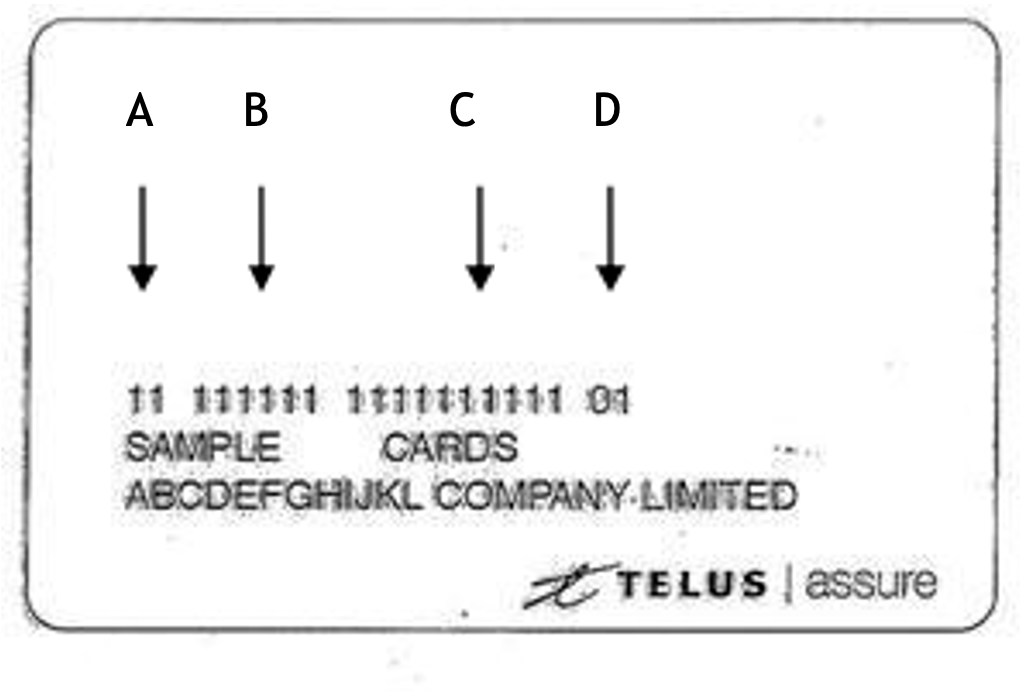
A - ID This is the identification number of the insurance carrier.
B - Policy Number This is the insured's policy number.
C - Certificate Number This is the insured's certificate number.
D - Issue Number Not applicable to dental plans (can be ignored).
Alberta Blue Cross
Canada Life (formerly Great West Life)
Green Shield

Group Medical Services
Groupe Premier Médicale
Medavie BlueCross
Quikcard


Pacific Blue Cross
Appendix B - DACnet Networks & Insurance Carrier Information
Click the link below for updated file for DACnet Networks and Supported Transactions, This document provides a detailed list of the types of transactions supported by the networks and insurance carriers on DACnet:
http://dacnet.ca/pdf/SupportedTransactions_DACnet_E_Jul29_2020.pdf
Appendix C - Patient Information Form

Appendix D – List of Error Codes
|
Error Code |
Message |
|
001 |
Missing/Invalid Transaction Prefix |
|
002 |
Missing/Invalid Dental Claim # or Office Sequence # |
|
003 |
Missing/Invalid Version Number |
|
004 |
Missing/Invalid Transaction Code |
|
005 |
Missing/Invalid Carrier Identification Number |
|
006 |
Missing/Invalid Software System ID |
|
007 |
Missing/Invalid Dentist Unique ID (Provider Number) |
|
008 |
Missing/Invalid Dental Office Number |
|
009 |
Missing/Invalid Primary Policy/Plan Number |
|
010 |
Missing/Invalid Division/Section Number |
|
011 |
Missing/Invalid Subscriber Identification Number |
|
012 |
Missing/Invalid Relationship Code |
|
013 |
Missing/Invalid Patient's Sex |
|
014 |
Missing/Invalid Patient's Birthday |
|
015 |
Missing Patient's Last Name |
|
016 |
Missing Patient's First Name |
|
017 |
Missing/Invalid Eligibility Exception Code |
|
018 |
Missing Name of School |
|
019 |
Missing Subscriber's Last Name or Name did not match to the one on file |
|
020 |
Missing Subscriber's First Name or Name did not match to the one on file |
|
021 |
Missing Subscriber's Address |
|
022 |
Missing Subscriber's City |
|
023 |
Missing/Invalid Subscriber's Postal Code |
|
024 |
Invalid Language of Insured |
|
025 |
Missing/Invalid Subscriber's Birthday |
|
026 |
Invalid Secondary Carrier ID Number |
|
027 |
Missing/Invalid Secondary Policy/Plan Number |
|
028 |
Missing/Invalid Secondary Division/Section Number |
|
029 |
Missing/Invalid Secondary Plan Subscriber Number |
|
030 |
Missing/Invalid Secondary Subscriber's Birthday |
|
031 |
Claim should be submitted to secondary carrier first (secondary is the primary carrier) |
|
032 |
Missing/Invalid Payee |
|
033 |
Invalid Accident Date |
|
034 |
Missing/Invalid Number of Procedures Performed |
|
035 |
Missing/Invalid Procedure Code |
|
036 |
Missing/Invalid Date of Service |
|
037 |
Missing/Invalid International Teeth or Sextant, Quadrant Arch Designation |
|
038 |
Missing/Invalid Tooth Surface |
|
039 |
Invalid Date of Initial Placement (Upper) |
|
040 |
Missing/Invalid Response re: Treatment Required for Orthodontic Purposes |
|
041 |
Missing/Invalid Dentist's Fee Claimed |
|
042 |
Missing/Invalid Lab Fee |
|
043 |
Missing/Invalid Unit of Time |
|
044 |
Message Length Field did not match length of message received |
|
045 |
Missing/Invalid E-Mail / Materials Forwarded Flag |
|
046 |
Missing/Invalid Claim Reference Number |
|
047 |
Provider is not authorized to Access CDAnet |
|
048 |
Please Submit Claim Manually |
|
049 |
No outstanding responses from the network requested |
|
050 |
Missing/Invalid Procedure Line Number |
|
Error Code |
Message |
|
051 |
Predetermination number not found |
|
052 |
At least one service must be entered for a claim/predetermination |
|
053 |
Missing/Invalid Subscriber's province |
|
054 |
Subscriber ID on reversal did not match that on file |
|
055 |
Reversal not for today's transaction |
|
056 |
Provider's specialty code does not match that on file |
|
057 |
Missing/Invalid response to Question "Is this an initial placement (Upper)" |
|
058 |
Number of procedures found did not match with number indicated |
|
059 |
Office Software is not certified to submit transactions to CDAnet |
|
060 |
Claim Reversal Transaction cannot be accepted now, please try again later today. |
|
061 |
Network Error, please re-submit transaction |
|
062 |
Missing/Invalid Payee CDA Provider Number |
|
063 |
Missing/Invalid Payee Provider Office Number |
|
064 |
Missing/Invalid Referring Provider |
|
065 |
Missing/Invalid Referral Reason Code |
|
066 |
Missing/Invalid Plan Flag |
|
067 |
Missing NIHB Plan fields |
|
068 |
Missing/Invalid Band Number |
|
069 |
Missing/Invalid Family Number |
|
070 |
Missing/Invalid Missing Teeth Map |
|
071 |
Missing/Invalid Secondary Relationship Code |
|
072 |
Missing/Invalid Procedure Type Codes |
|
073 |
For Future Use |
|
074 |
Date of Service is a future date |
|
075 |
Date of Service is more than one year old |
|
076 |
Group not acceptable through EDI |
|
077 |
Procedure Type not supported by carrier |
|
078 |
Please submit pre-authorization manually |
|
079 |
Duplicate claim |
|
080 |
Missing/Invalid Carrier Transaction Counter |
|
081 |
Invalid Eligibility Date |
|
082 |
Invalid Card Sequence/Version Number |
|
083 |
Missing/Invalid Secondary Subscriber's Last Name |
|
084 |
Missing/Invalid Secondary Subscriber's First Name |
|
085 |
Invalid Secondary Subscriber's Middle Initial |
|
086 |
Missing Secondary Subscriber's Address Line 1 |
|
087 |
Missing Secondary Subscriber's City |
|
088 |
Missing Secondary Subscriber's Province/State Code |
|
089 |
Invalid Secondary Subscriber's Postal/Zip Code |
|
090 |
Missing/Invalid response to Question: Is this an Initial Placement Lower |
|
091 |
Missing/Invalid Date of Initial Placement Lower |
|
092 |
Missing/Invalid Maxillary Prosthesis Material |
|
093 |
Missing/Invalid Mandibular Prosthesis Material |
|
094 |
Missing/Invalid Extracted Teeth Count |
|
095 |
Missing/Invalid Extracted Tooth Number |
|
096 |
Missing/Invalid Extraction Date |
|
097 |
Invalid Reconciliation Date |
|
098 |
Missing/Invalid Lab Procedure Code |
|
099 |
Invalid Encryption Code |
|
100 |
Invalid Encryption |
|
101 |
Invalid Subscriber's Middle Initial |
|
102 |
Invalid Patient's Middle Initial |
|
Error Code |
Message |
|
103 |
Missing/Invalid Primary Dependent Code |
|
104 |
Missing/Invalid Secondary Dependent Code |
|
105 |
Missing/Invalid Secondary Card Sequence/Version Number |
|
106 |
Missing/Invalid Secondary Language |
|
107 |
Missing/Invalid Secondary Coverage Flag |
|
108 |
Secondary Coverage Fields Missing |
|
109 |
Missing/Invalid Secondary Sequence Number |
|
110 |
Missing/Invalid Orthodontic Record Flag |
|
111 |
Missing/Invalid First Examination Fee |
|
112 |
Missing/Invalid Diagnostic Phase Fee |
|
113 |
Missing/Invalid Initial Payment |
|
114 |
Missing/Invalid Payment Mode |
|
115 |
Missing/Invalid Treatment Duration |
|
116 |
Missing/Invalid Number of Anticipated Payments |
|
117 |
Missing/Invalid Anticipated Payment Amount |
|
118 |
Missing/Invalid Lab Procedure Code #2 |
|
119 |
Missing/Invalid Lab Procedure Fee #2 |
|
120 |
Missing/Invalid Estimated Treatment Starting Date |
|
121 |
Primary EOB Altered from the Original |
|
122 |
Data no longer available |
|
123 |
Missing/Invalid Reconciliation Page Number |
|
124 |
Transaction Type not supported by the carrier |
|
125 |
Transaction Version not supported |
|
997 |
Last Transaction Unreadable |
|
998 |
Reserved by CDAnet for future use |
|
999 |
Host Processing Error - Resubmit Claim Manually |
Note: Not all error codes will apply to your version of DACnet; this list is intended for reference only.
Appendix E - Patient Authorization Labels
The following two pages are sample sheets, which you can use to create labels for insertion in your files. The patient must provide your office with his or her authorization for claims to be sent electronically and for any assignment of benefits you undertake. You may wish to obtain this authorization using a central logbook, or with individual labels such as these.